
ETPOC is the preferred provider of prosthetic services in Longview and is well known for attention to detail and exceptional patient services. Some of our patients travel several hours to receive the level of care offered by our staff. We understand that each patient is unique and requires individualized attention to meet specific needs. Our staff has years of experience and is equipped to treat and provide prosthetic services to patients of all age groups. We interact with our patients in multiple medical environments – not exclusive to – hospitals, rehab-centers, physician offices and our own patient care facility.
Offering unparalleled service throughout East Texas, ETPOC is experienced in designing, fabricating, and fitting prostheses for any age group and level of amputation. As clinical practitioners our staff practitioners have been exposed to a variety of congenital deformities and are highly qualified to treat any pediatric prosthetic patient.
Prescription recommendations specifying the most functional and cost effective systems are developed based on the patient’s age, activity level, special needs, and rehabilitation potential. Lower extremity prostheses include ultralight and energy storing designs for geriatric or athletic patients, plus custom socket (patient residual limb interface) design and a variety of suspension systems.
ETPOC specializes in partial foot prostheses, cosmetic coverings, and hybrid prosthetic designs. In addition to treating lower extremity patients, ETPOC is equally adept at designing, fabricating, and fitting body powered, myoelectric, and switch controlled upper extremity prostheses.
Prosthetic needs begin prior to or following your amputation. Our clinicians routinely consult with patients and their surgeons prior to scheduled surgeries in order to discuss amputation levels that are most beneficial for post-surgical prosthetic use and function.
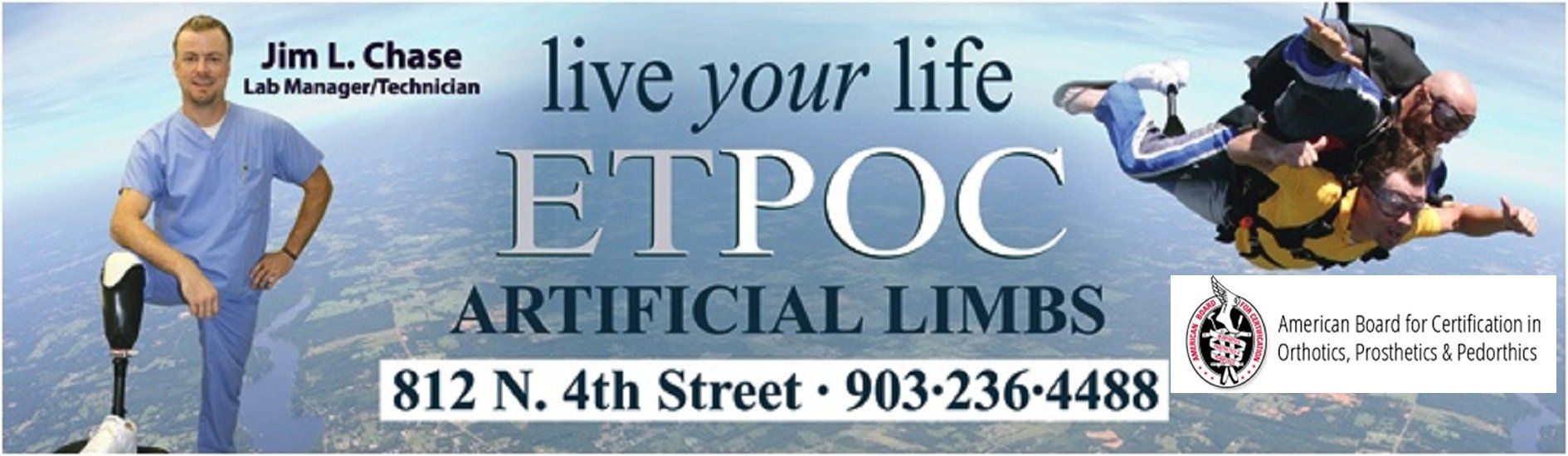
Mr. Jim Chase, ETPOC’S technical director, often visits patients prior to and immediately following surgery and considers it his mission to offer peer support for those in need. In the event you have not been introduced to our practice prior to surgery, ETPOC clinicians are available for consultations, post-operative supplies and educational materials upon receipt of physician orders. If you are discharged from the hospital your surgeon may refer you to us during a follow up visit.
Patients not yet referred to a prosthetist may contact our office at 903-236-4488 and schedule an appointment.
NEW AMPUTEE TREATMENT PLAN
Undergoing an amputation is a life changing experience that leaves patients and families with many questions about the future. It is normal to feel different emotions of depression, helplessness, anger, and anxiety of what your life will be like, living with limb loss. It doesn’t matter whether it was a traumatic amputation or caused by health related issues, nothing can prepare you for the feelings you may have.

One of our goals is to help you through this process by teaching you and your family about prosthetic services and the steps leading up to receipt of your prosthesis. Our licensed and certified prosthetists have years of experience and can provide valuable guidance and education.
ETPOC’s Technical Director Jim Chase, an amputee himself, has been instrumental in offering peer support for new patients and their families. Mr. Chase and numerous current patients are available for you and your family to share with you their experience and assist in guiding you through this process.
For more information about our amputee peer support or a prosthetic consultation, please complete the an inquiry form at the bottom of the page or feel free to call us.

It is important to understand the role the rehab team plays in your recovery. The team consists of your surgeon or family physician, your physical therapists, your prosthetist, yourself and family. Not every amputee has this team of professionals assisting them, but we encourage you to try to establish one.
Your physician or surgeon will be instrumental in prescribing your prosthesis, providing all referrals and for Rehabilitation Therapies, and providing proper and necessary documentation for insurance purposes. In most cases your surgeon will continue follow-up care as you engage and complete initial Physical Therapy prosthetic gait training, the process of learning to use your prosthesis. Your physician will follow up with you routinely to make sure you are progressing according to your prosthetic rehabilitation treatment plan and at times will need to prescribe adjustments or supplies for your prosthesis.
A prosthetists is a person who measures, designs, fabricates, fits, or services a prosthesis as prescribed by a physician. Your prosthetist will help determine what type of prosthesis would be appropriate for you based on your activity level, health status, hobbies and occupation. We provide all services related to the prosthesis and supplies needed to make it fit well and function properly. It is relationship that can last many years, as a prosthesis is a tool that periodically needs to be adjusted and replaced.
Physical Therapists are instrumental in teaching a new amputee how to walk with their prosthesis. Prosthetic Gait Training is a type of physical therapy that helps people improve their ability to stand and walk with a prosthesis. Following receipt of your prosthesis, Physical Therapy can be provided by home health care professionals or at an out-patient rehabilitation facility. Prosthetic and rehabilitation patients usually receive physical therapy three times weekly in order to obtain independent while resuming normal daily activities. While working with both your prosthetist and Physical Therapist you will learn how to care for your prosthesis and what’s involved in maintaining it on a daily basis. ETPOC is a strong proponent of Physical Therapy and believe it to be one of the key factors affecting successful use of a prosthesis.
The more you know about the rehabilitation process and prosthetics, the more successful you will be with your new prosthesis.
One of the most difficult problems facing a new amputee is edema, or swelling of the residual limb. The care you give your residual limb initially will directly affect your success with your new prosthesis. Upon healing your prosthetist will take a measurement of your residual limb and fit you with a prosthetic shrinker. While a typical amputation heals within 6 weeks after surgery allowing the use of a shrinker, some patients with severe circulatory compromise or uncontrolled diabetes may experience a delay.
 The shrinker is used to reduce edema (swelling) of the residual limb in preparation for casting, impressions, and measurements necessary to manufacture your prosthesis. Shrinker use prior to casting typically spans a three to four week period in which you will be fit with several smaller shrinkers as you experience reduced limb edema. Use of a prosthetic shrinker will continue after receipt of your prosthesis in order to maintain volume stability and allow a more accurate fit of your prosthesis.. This is especially important for dialysis patients and those experiencing fluctuations in residual limb volume. You will use your shrinker 24 hours a day, except when exercising, bathing, or while using your prosthesis.
The shrinker is used to reduce edema (swelling) of the residual limb in preparation for casting, impressions, and measurements necessary to manufacture your prosthesis. Shrinker use prior to casting typically spans a three to four week period in which you will be fit with several smaller shrinkers as you experience reduced limb edema. Use of a prosthetic shrinker will continue after receipt of your prosthesis in order to maintain volume stability and allow a more accurate fit of your prosthesis.. This is especially important for dialysis patients and those experiencing fluctuations in residual limb volume. You will use your shrinker 24 hours a day, except when exercising, bathing, or while using your prosthesis.
Proper hygiene is essential. Wash your limb thoroughly with soap and water every day, unless your doctor has instructed you otherwise. Sometime, people have sensitive or painful spots on their residual limb or along the suture line. Deep tissue message following healing of your residual limb is often recommended in order to reduce sensitivity or "desensitize" problem areas. Improving tolerance to touch or slight pressure helps decrease limb sensitivity and sometimes reduces the feelings of itching, pain or "Phantom Limb Sensation or Pain" which refers to sensations radiating from the missing limb.
Physical therapy to regain strength and agility is an important step in your preparation to use your new prosthesis. You may have had some therapy while you were in the hospital, and chances are your doctor will want you to continue with it, both now and after you receive your new prosthesis. The strength you develop now will help you to walk as normally as possible in the future. Your doctor, prosthetist and physical therapist will work together, or independently, to evaluate when you are ready to be cast for your prosthesis.
ETPOC will work with you, your physician and/or physical therapist to design a prosthesis that is right for you. Prosthetic recommendations are based on the progress made in Physical Therapy and your K Level as determined by a your doctor, physical therapist, and prosthetist. The standardized AmPro (amputee mobility predictor) is a test administered by a physical therapist used to determine your K Level (current and potential activity level). The score obtained on the AmPro helps determine optimal component selection and design of your prosthesis. Our goal is to fabricate a custom prosthesis as close to your natural limb as possible in appearance and function. We use high strength, lightweight materials which will be designed to match your leg in size, shape, and even skin tone. Your prosthetic foot will be responsive enough to provide motion for a natural-looking gait.
An appointment for casting will be scheduled after it has been determined that the volume and size of your residual limb has stabilized.  Our prosthetist and technicians will use a cast of your residual limb to make a temporary diagnostic test socket utilized to determine the fit and alignment of the prototype system.
Our prosthetist and technicians will use a cast of your residual limb to make a temporary diagnostic test socket utilized to determine the fit and alignment of the prototype system.
 Your prosthetist will spend a lot of time working with you during the test socket fitting to make sure your prosthesis is adjusted perfectly to your needs and comfort. The alignment fitting will take into account every aspect of your prosthesis’ fit and function. A lot of attention will be focused on the socket shape because it needs to spread out the pressures on your residual limb evenly and comfortably when you walk on it. The alignment is important to make sure your knee and hip are straight when you stand and walk, and the height of the prosthesis is not too tall or short. Following successful test socket fitting you will receive your initial prosthesis within a one week period. Following receipt of your initial prosthesis you will commence Physical Therapy prosthetic gait training while continuing rehabilitation.
Your prosthetist will spend a lot of time working with you during the test socket fitting to make sure your prosthesis is adjusted perfectly to your needs and comfort. The alignment fitting will take into account every aspect of your prosthesis’ fit and function. A lot of attention will be focused on the socket shape because it needs to spread out the pressures on your residual limb evenly and comfortably when you walk on it. The alignment is important to make sure your knee and hip are straight when you stand and walk, and the height of the prosthesis is not too tall or short. Following successful test socket fitting you will receive your initial prosthesis within a one week period. Following receipt of your initial prosthesis you will commence Physical Therapy prosthetic gait training while continuing rehabilitation.
When the prosthesis is finished, a final delivery appointment will be scheduled. It is common for this final fitting to occur in the office however, this can take place at rehabilitation facilities or the patient’s home. The prosthesis will be evaluated one final time for comfort and alignment.
It is important that you learn to walk properly with your new prosthesis from the day you receive it. Your physical therapist will work with you and make recommendations regarding any additional support you may need to walk your best – such as a walker, crutches, or a cane. With your therapist’s help, you will soon be accomplishing many of your daily activities. We will be counting on you to call us whenever you have any questions about the fit, alignment, or general performance of your prosthesis. We are members of your team, and want to help you do your best now and in the future.
Most new amputees experience atrophy and shrinking of the residual limb. This is perfectly natural, but it does affect the fit of your prosthesis. Adjustments to the fit of your prosthesis are made by using prosthetic socks of varying ply and thicknesses. Throughout rehabilitation and continued use of a prosthesis ETPOC will schedule you for regular follow-up visits in order to monitor the fit and function of your prosthesis. While wearing a prosthesis new amputees go through many changes in the size and shape of their residual limb during the two year period following surgery. It is very important that you attend scheduled appointments allowing our staff to assess these changes and inspect the use of prosthetic socks used to adjust the fit of your socket.
Our staff will always be upfront and honest with you regarding your insurance coverage and your financial responsibility. If you are uninsured, and in most cases want to return to work, ETPOC will assist you in seeking funding sources available for prosthetic services.
UPPER EXTREMITY PROSTHETICS
![]()
Patients missing all or part of an arm is less common than lower extremity limb loss. Most upper extremity prosthetic patients encountered at ETPOC are victims of trauma, cancer, or congenital conditions. Our staff is experienced in all types of upper extremity design and strive to fit each and every patient with the most appropriate system. Variables such as your functional abilities, vocational and recreational needs as well as preference of cosmetic finish provide our staff important information allowing ETPOC to design and provide you optimal upper extremity services.

Our goal is to help you function to the best of your ability with a prosthesis that is as effective, durable and as comfortable as possible. Your prosthetist, doctor and occupational therapist will help you through the following steps to return to an active lifestyle with your new prosthesis.

Upon healing your prosthetist will take a measurement of your residual limb and fit you with a prosthetic shrinker. While a typical amputation heals within 6 weeks after surgery allowing the use of a shrinker, some patients with severe circulatory compromise, excessive scarring due to trauma or uncontrolled diabetes may experience a delay.
The shrinker is used to reduce edema (swelling) of the residual limb in preparation for casting, impressions, and measurements necessary to manufacture your prosthesis. Shrinker use prior to casting typically spans a three to four week period in which you will be fit with several smaller shrinkers as you experience reduced limb edema. Use of a prosthetic shrinker will continue after receipt of your prosthesis in order to maintain volume stability and allow a more accurate fit of your prosthesis.. This is especially important for dialysis patients and those experiencing fluctuations in residual limb volume. You will use your shrinker 24 hours a day, except when exercising, bathing, or while using your prosthesis.
The main objectives in upper extremity prosthetics are to meet vocational, recreational and general lifestyle needs of each amputee and to achieve an aesthetically pleasing outcome. This makes prosthetic management for upper extremity amputees a highly individualized process.
Occupational therapy to regain strength and fine motor function is an important step in preparation for using an upper extremity prosthesis. Therapy should begin during your hospital stay and continue upon your discharge prior to and following fitting of your prosthesis. The strength and coordination you develop during occupational therapy will help assure optimal functional use of your prosthesis.
While new technology has greatly expanded the component selection available for patients all upper extremity prosthetic devices fall into simple categories. Passive prostheses are generally considered to be devices that are worn purely for cosmetic purposes and do not provide functional restoration. The passive prosthesis is not usually considered medically necessary and therefore typically not covered through a patient's insurance coverage. Functional prostheses, on the other hand, are devices that enable an amputee to perform tasks. These devices may or may not also serve a cosmetic purpose. Functional prostheses are classified according to the method of operation and consist of body powered, externally powered systems, or a combination of body and externally powered (hybrid system).
BODY POWERED PROSTHESES (Conventional)
Body-powered upper extremity prostheses are the most common type of upper limb prostheses. It allows the prosthetic user to control the terminal device (usually a hook or a hand) and/or elbow in the case of above elbow systems via a harness system that fits around the chest and shoulder. This type of prosthesis is very reliable and can be used in environments involving dust and water.
EXTERNALLY POWERED PROSTHESES
Externally powered upper extremity prostheses use a battery powered electric motor to control the terminal device, eliminating the need of a harness system. Sensors in the form of electrodes or switches, embedded in the socket, pick up an electrical or mechanical signals on the skin which are transferred to a processor controlling the functions of the motor. Intensive training is essential to ensure a successful outcome.
HYBRID SYSTEMS
Hybrid systems are a combination of externally and body powered prostheses. This type can be used for Transhumeral (above-elbow) amputees, providing functional restoration of elbow and hand. Usually, the elbow joint is controlled via a harness system and the terminal device is controlled through an external power source, for example myo-electrically.
In most cases ETPOC recommends the use of a body powered prosthesis for new amputees. The body powered system is utilized by the new amputee as an initial prosthesis allowing continuation of therapy, rehabilitation, and management of residual limb atrophy. As a new amputee, you will experience limb size reduction which would have a negative impact on the fit and function of the externally powered system which relies on consistent limb size and skin contact with electrodes placed in the socket. Upon reaching residual limb size stabilization while using your body powered system, our staff will visit with you to determine the most appropriate externally powered prosthesis to meet your functional needs and expectations.
Body-Powered or Electric-Powered Prosthesis?
When choosing between a body-powered or electric-powered prosthesis, you should carefully consider the advantages and disadvantages of each.
Advantages of Body-Powered Devices
• Lower Initial Cost
• Lighter
• Easier to repair
• Offer better tension feedback to the body
Disadvantages of Body-Powered Devices
• Mechanical appearance
• Difficult to use for some people because they depend on the user’s physical ability
Advantages of Externally Powered Devices
• May not require a harness and can, therefore, be built to look more like a real arm
• Battery-powered so body strength and body movement are not as important for their operation
• Provide a strong grip force
Disadvantages of Externally Powered Devices
• Higher initial cost
• Heavier (Improved batteries have, however, helped reduce their weight and increase their capacity and voltage.)
• Higher repair cost
• Dependence on battery life
• Electric components may be affected by environmental conditions causing failure
A major improvement in externally powered upper extremity prostheses is the use of multiple methods of control. Externally powered prostheses are not exclusively myoelectrically controlled. Myoelectric systems incorporate multiple electrodes in contact with the patient's skin which receive electrical impulses from activated muscles used to control the speed and direction of the prosthesis. In addition to myoelectrics, other forms of externally powered control systems include pressure switches, harnesses, and positional servo devices.
In many cases today's prostheses are designed with more than one kind of control system for a prosthesis. For example, a prosthesis may include myoelectrodes to control the hand and a positional servo transducer to control the elbow, offering independent and simultaneous control. In the past, operation of an upper extremity prosthesis required that operation involved one action at a time or sequentially. Historically above elbow amputees were unable to flex and extend the elbow while simultaneously using the terminal device however, with the advent of the multiple input concept, patients are given the ability to operate multiple features concurrently, therefore, have smoother, simultaneous movements.
Demo Content
Demo Content
It is important that you learn to use your new prosthesis properly from the day you receive it. Upper extremity prosthetic patients typically engage in occupational therapy in order to learn how to use a prosthesis. Your occupational therapist will work with you to perform tasks of daily living such as buttoning a shirt, holding utensils, and opening a jar. With your therapist’s help, you will soon be accomplishing many of your daily activities. It is important that you contact our office whenever you have questions regarding the fit, comfort or general performance of your prosthesis. As members of your team we want to assist you in every way possible so that you achieve optimal use and function of your prosthessis.
Demo Content
